HSC1103 – Radiobiology and Radiation Protection – Radiation Protection
- Oct 21, 2018
- 7 min read
Learning Objectives
Principles of radiation protection
Justification
Optimisation
Limitation
International organisations, National regulatory agencies
Beam attenuation properties
Shielding considerations
Radiography
Radiation therapy
Management of radiation incidents – accidents / misplaced sources / spillages
This chapter will cover the rationale and goals for radiation protection, along with the four quartets of radiation protection. We will also take a look at some radiation protection organisations on a local and international level, and learn to identify the local regulatory authority for radiation protection and discuss the regulatory requirements, and also four major responsibilities of the medical radiation professional. We will then examine the general principles for room shielding, and define a radiation accident and the subsequent necessary action for follow-ups.
Goal of Radiation Protection
The two goals of radiation protection are:
To prevent deterministic effects completely – by keeping radiation doses below threshold values
To minimize the probability of stochastic effects – by taking all reasonable efforts to keep doses low
It is so phrased because it is possible to eliminate deterministic effects completely; they are dose dependent. This means that we just need to keep doses below the threshold value. However, when stochastic effects were discovered to present themselves regardless of a threshold value, following the LNT model, the next goal is to keep the probability of stochastic effects as low as possible.
The ICRP (International Commission on Radiological Protection) is guided by three fundamental principles:
Justification – Any exposure of a patient to radiation should result in more benefit than harm.
Optimisation – All exposures should be kept as low as reasonably achievable, taking into account economic and social factors.
Limitation – The exposure of individuals should not exceed the limits recommended for the appropriate circumstances.
The four quartets of radiation protection are as follows:
Personal actions – time, shielding, distance
Department activities – control access shield, monitoring, training
Administrative structure – laws, regulations, licensing, accreditation
Philosophy – justification, optimizing, limitation
Every radiation worker monitors their occupational dose of radiation. In Singapore, this is done with the thermoluminescent dosimeter (TLD), and the report is generated by NEA (National Environmental Agency) every 3 months.
The maximum allowed dose to whole body is 20mSv/year averaged over a period of 5 consecutive years, with no more than 50mSv in any one year. This is NEA’s way of keeping the stochastic effects as low as possible.
For deterministic effects, the maximum equivalent dose allowed for the lens of the eye is 150mSv/year, and the dose allowed for skin and extremities is 500mSv/year. Local regulations also stipulate that no individual below the age of 18 years shall engage in radiation work.
A summary for yearly limits can hence be shown, as such:
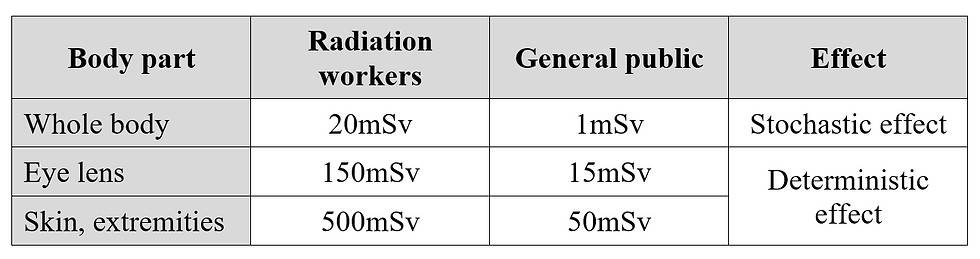
In Singapore, the average member of the general public receives about 1mSv of radiation dose annualy. This is broken down into its various sources as shown:

Responsibilities of a medical radiation professional
In order to protect the patient, personnel, and members of the public, a medical radiation professional’s responsibilities include:
Responsibility to the patient
Responsibility to oneself as a radiation worker
Duty to continuing education
Responsibility in dose optimization in the effective application of the ALARA principle
It is also important to look at professional values and think of how they relate to a medical radiation professional’s perspective.
To exercise dignity, it is important to practice informed consent and ensure that patients understand the procedures they’re about to be subjected to.
To exercise nonmaleficence/beneficence, it is necessary to follow the 3 fundamental principles of justification, optimization and staying within the dose limits.
To exercise justice, it is necessary to measure the dose prescribed to the dose limits.
To maintain prudence and precaution, it is necessary to conform to the linear no-threshold model of radiation response.
In order to maintain integrity, we need to know the importance of patient education.
There are several international bodies that govern radiation protection.
ICRP – International Commission on Radiological Protection
ICRU – International Commission on Radiological Units and Measurements
IAEA – International Atomic Energy Agency
UNSCEAR – United Nations Scientific Committee on the Effects of Atomic Radiation
BEIR – Biological Effects of Ionising Radiation Committee
Locally, the NEA – National Environmental Agency is the national authority for Radiation Protection.
The RPNSD – Radiation Protection & Nuclear Science Department of the NEA, administers and enforces the Radiation Protection Act and the ionizing radiation regulations through a system of licensing, notification, authorization, inspection and enforcement.
Shielding
The Half Value Layer (HVL) is the thickness of attenuation material that reduces the original intensity of the radiation by half.
The equation relating intensity to thickness of shielding material is given as such:

μ represents the attenuation coefficient, and I_0 is the initial intensity of the beam. x is the thickness of the attenuating material.
Since the HVL attenuates half the intensity of the beam,

The HVL of some of the common attenuating material is shown here:

Lead is the standard material used for x-ray walls, and is applied to the room’s internal walls.
The design of the walls also matter. Sliding doors are better than push doors as they are tighter in terms of radiation shielding.
Licensing for x-ray measuremenets is performed at the maximum continuous tube current, 3mAs ~ 5mAs, and at 150kVp. Local regulations state that “nowhere outside the x-ray room accessible to any individual shall have a radiation level exceeding 10μSv/hr while the x-ray machine is being operated at its maximum rated current for the maximum rated voltage and at its normal operation positions.”
Primary radiation is the radiation that has emerged from the x-ray tube that has yet to be attenuated, thus requiring a primary barrier. The primary barrier is located perpendicular to the undeflected line of travel of the x-ray beam. Secondary radiation includes scattered and leakage radiation, and requires a secondary barrier. The walls that are not in the direct line of travel of the primary beam are called secondary protective barriers.
A controlled area is defined as a limited-access area in which the occupational exposure of personnel to radiation-producing equipment or radioactive materials is supervised by a designated individual – like an L5 or L6 license holder. Examples of controlled areas include the treatment room or x-ray room, or the control console.
An uncontrolled area includes any other area not designated as a control area environment. Examples of these include lobbies, offices, waiting areas, consultation rooms and rest rooms.
Workload factor
In diagnostic radiography facilities, the workload is defined as the milliampere minutes of beam on time per week, and is calculated by multiplying the number of patients per week by mAs per patient.
For example, if a chest x-ray room handles 12 patients per hour with 10mAs per patient, this works out to be 120 mAs per hour, and 4800 mAs per week. Converting to the correct units, this room has a workload of 80 mAmin/wk. In radiation therapy, the unit is defined as cGy/wk.
The Use Factor is the fraction of operating time during which the radiation is directed towards a particular barrier. This only applies to primary beams, and roughly follows as such:
Floor: 1 (for single fields)
Ceiling (bucky): 1/4
Ceiling (C-arm): 1/2
Walls: 1/4
The use factor of secondary barriers is always 1, because leakage and scatter radiation is always present when the tube is energized.
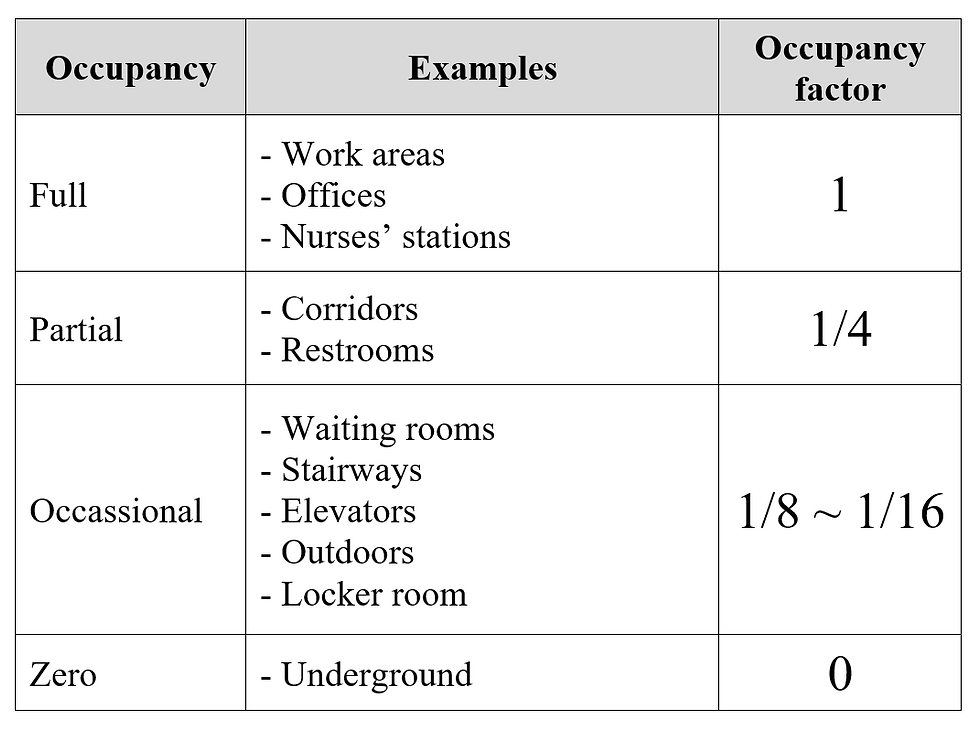
The Occupancy factor is the fraction of time that the space to be shielded is occupied. It is always 1 for all controlled areas. The possible future usage of the space around the x-ray / treatment room must be considered during the planning process. The occupancy factor of various types of places are shown below:
Distance is also another important factor. By the inverse square law, the intensity of the radiation decreases by the distance squared. This means that distance is the most effective way in reducing radiation intensity.
260cm of concrete is usually sufficient as a primary barrier for a machine running up to 18MV photons. The secondary barriers would also be concrete, and would be 130cm thick.
With all these precautions and factors in place, it is still important to remember that shielding calculations are conservative, and that calculated shielding values need to be larger than what is required for radiation protection, so as to combat “worst-case” scenarios.
For example,
The field size and phantom size used for scatter calculations are up to 4 times higher than those typically used
High occupancy periods are used within an uncontrolled area
Materials in the x-ray room that could contribute to reducing radiation transmission such as mobile lead screens are not included in calculations
There are also a multitude of safety devices in radiation treatment rooms. One such safety device is the door interlock. The radiation beam is required to turn off when the circuit is interrupted. During an interlock, only a deliberate action by the operator can allow the system to resume treatment.
There are also safety edges which stops the door from continuing to close when it hits something. Warning lights are also very prevalent and are required at the entrances to treatment rooms.
Reporting of Radiation Incidents
The definition of a radiation incident is as follows: A misuse of irradiating apparatus or maladministration of a radioactive material for medical purposes, including:
Any therapeutic treatment delivered
To the wrong patient of to the wrong tissue of any patient
Using the wrong radiopharmaceutical
With a dose or dose fractionation which differs by more than 10% from the value prescribed by medical practitioners, or which may lead to acute effects
Any diagnostic exposure greater than 50% of the intended dose or resulting in doses repeatedly or substantially exceeding the established normal doses for diagnostic radiological examiniations
Any equipment failure, error, mishap or other unusual occurrence which has the potential to cause a patient to receive a dose significantly different from that intended
If any radiation incident should occur, the L5 or L6 licensee has to notify the appropriate authority, in local context this is MOH and RPNSD.
A preliminary oral report of the incident within 24 hours
Confirmed in writing within 48 hours
Full written report of the accident within 10 days














Comments